The school itself shall be made a genuine form of active community life, instead of a place set apart in which to learn lessons.— John Dewey, School and Society (1907)



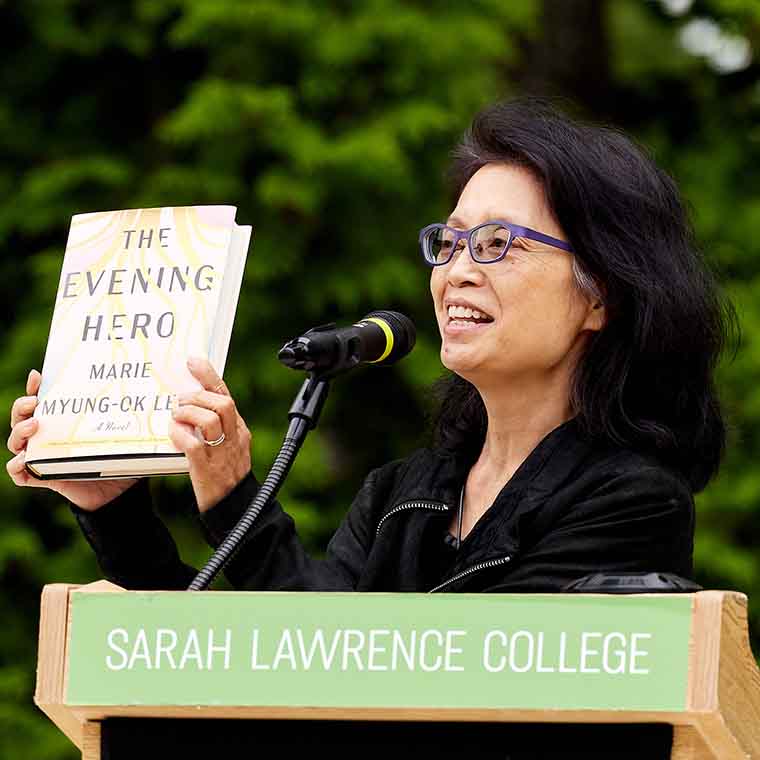
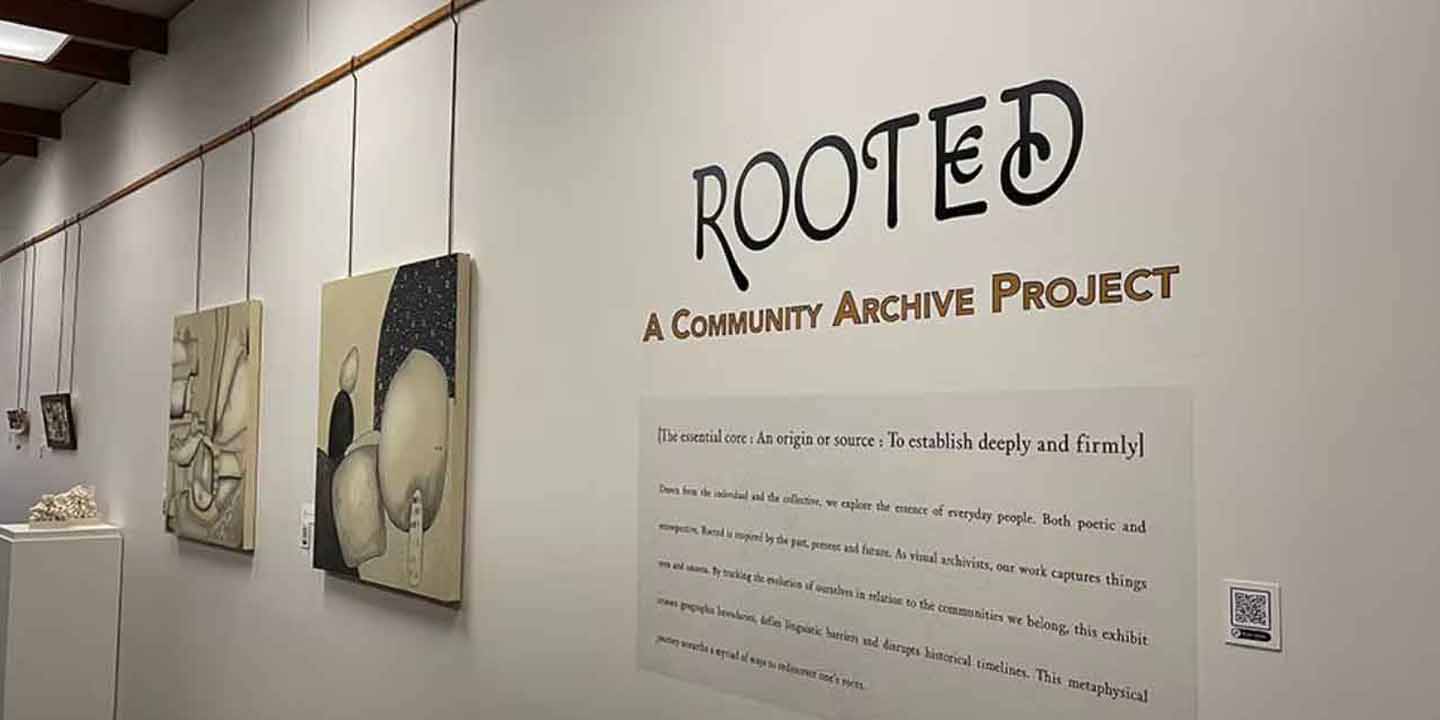
Creative and Performing Arts
The synergistic dynamic between our undergraduate, graduate, and lifelong learning programs allows for intergenerational connections and artistic collaborations. The College intentionally works to further these relationships through community collaborations such as Theatre & Civic Engagement programming in the performing arts. The Writing Institute provides non-credit creative writing classes for adults, online and on campus. The Writing Institute also cultivates teaching artists from the College’s MFA in Writing Program to help young writers hone their craft through pre-college programming in partnership with Yonkers Public Schools, community based organizations, and the summer Writers’ Week program.




Children, Childhood, and Education
Through our Children, Childhood, and Education Collaborative, Sarah Lawrence promotes progressive education and a philosophy of the learning child as the maker of their own meaning, emphasizing curiosity and exploration as the foundations for lifelong learning. At the Early Childhood Center, our laboratory preschool and kindergarten, the concept of strengths perspective is put into practice; children are at the center of their education and celebrated for their uniqueness. The Child Development Institute advances this pedagogy through thought leadership, professional development programming for teachers, and Community Adventure Play Experiences for children and families. Similarly, our Center for the Urban River at Beczak, located on the banks of the Hudson River, offers members of our surrounding communities a rich understanding of their environmental impact by providing a plethora of experiential learning opportunities.




Health Sciences and Society
As the first institution to offer graduate degrees in genetic counseling and Health Advocacy, the College has a long legacy of innovation and promoting evolution in the health sciences and society sector. One in five genetic counselors is an alum of the Joan H. Marks Graduate Program in Human Genetics and many more will soon join our community by taking part in professional development offerings through our nascent Institute for Genomics Education, Workforce & Leadership. We’ve similarly launched new, asynchronous certificate programs in Health Advocacy to enable maximum flexibility of enrollment for healthcare professionals and aspiring patient advocates.



Civic Engagement & Experiential Learning
Through collaborative work with a diverse array of organizations and support from the Mellon Foundation, our students deepen their humanistic values and concern for the community while also making impactful contributions across Westchester County and New York City. These experiences are supported through the offices of Community Partnerships & Engagement and Embedded Education. As an institution, we have established similar reciprocal relationships through initiatives such as our Westchester Community College Transfer Agreement, Mellon Grant for Civic Engagement, and the Sarah Lawrence Interdisciplinary Collaborative on the Environment (SLICE).